Are you processing payer authorization responses efficiently?
On-demand webinar
According to a 2022 American Hospital Association (AHA) survey, 95% of hospitals and health systems report increased staff time spent seeking authorization approval.*
This webinar is for you if you are:
- Managing thousands of e-faxes or hard faxes from payers
- Transcribing Bed Day Table authorization information into your EMR
- Processing payer faxes into a records system
We gathered a panel of industry leaders to share how they've optimized workflows and improved efficiency in processing payer responses for authorizations.
Complete this form, and we'll send you a link to view the on-demand webinar.
Our Panelists
Dr. Robert Bolash
Medical Director, Cedars-Sinai
Joy LaGuardia
MSN, RN, BSN, CCM
Systems Manager for Transitions of Care & Clinical Authorization Review Division, UCLA Health
Russell Graney
CEO & Founder, Aidin
Download the on-demand version now
What you'll hear in this webinar
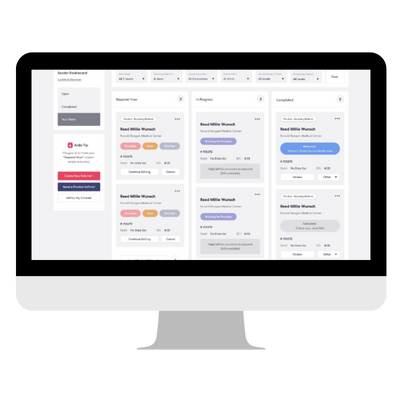
- Hear our panelists discuss lessons learned and tips based on their experience optimizing their UM workflows around payer responses by leveraging AI-based technology and process improvements.
- Learn how top organizations like Cedars Sinai and UCLA are streamlining inbound responses from payers on authorizations and reducing the time and administrative burden on their case managers.
- Understand how to define and measure key outcomes and objectives for UM and case management optimization projects.
- Get tips to prioritize optimization opportunities in common UM and case management workflows.
*Source: AHA November 2022 Survey